Key takeaways
- Fair scheduling reduces burnout through data-driven tools with equity and balanced workloads, improving well-being and patient care.
- Automation reduces planning and schedule creation by up to 98%, freeing staff from manual, error-prone processes.
- Giving physicians autonomy and secure, real-time communication tools leads to higher satisfaction and fewer care disruptions.
Effective physician scheduling in healthcare organizations is crucial to ensuring a collaborative ecosystem where patient needs come first.
But in practice, manual schedule creation causes undue administrative burden. This causes staff dissatisfaction due to inefficient shift distribution, and patient dissatisfaction through prolonged wait times. The good news is these challenges and the impact they have on access to care, patient well-being, and care provider work-life balance can be mitigated. But first, let’s dive into the five most common physician scheduling challenges:
- Promoting work-life balance
- Navigating absences and last-minute changes
- Overcoming administrative burden
- Limiting communication errors
- Supporting physician autonomy
Challenge 1: Promoting work-life balance
Manual scheduling processes often lack the insight to allocate shifts equitably, because they rely on subjective judgements. Uneven workloads can lead to physician burnout and compromised patient care.
According to the Medical Group Management Association, 80% of healthcare leads report their level of stress or burnout increased in 2022[1], and 56% of physicians say scheduling challenges severely limit work-life balance.[2] The increasing intensity of physician workload in healthcare organizations is a significant issue, impacting individual performance, absenteeism, turnover, and organizational performance. Healthcare professionals, including physicians, were , exposing them to significant physical and psychological distress. Additionally, despite the increasing significance of primary care, there is a notable decline in the number of general practitioners (GPs) and widespread discontentment among them in various countries. during the COVID-19 crisis, exposing
Green, Christian (2022, September 7). Stress and burnout a growing concern for healthcare leaders. MGMA. https://www.mgma.com/mgma-stats/stress-and-burnout-a-growing-concern-for-healthcare-leaders
CMA (2022, November 15). Physician wellness: New 2021 National Physician Health Survey findings — burnout, short-staffing and an overburdened system take their toll. Canadian Medical Association. https://www.cma.ca/physician-wellness-hub/content/physician-wellness-new-2021-national-physician-health-survey-findings-burnout-short-staffing-and them to significant physical and psychological distress. Additionally, despite the increasing significance of primary care, there is a notable decline in the number of general practitioners (GPs) and widespread discontentment among them in various countries.
To address this challenge, healthcare organizations use innovative solutions like equity counters. These ensure schedules are fair across teams by measuring against the “weight” of each task or shift to highlight potential issues. By leveraging data-driven insights, the equity counter considers factors such as patient demand, physician availability, and skill sets to recommend optimized schedules.
Fairly distributed workloads for night shifts, weekends, and on-call duties lead to better physician experiences and higher job satisfaction. These positive impacts lead to healthier relationships between colleagues and better care delivery.
Challenge 2: Navigating absences and last-minute changes
Last-minute changes and shift swaps in physician schedules cause significant disruptions within care facilities. The difficulty lies in finding suitable replacements quickly and ensuring patient appointments and procedures are maintained.
This process is time consuming, manual, and not very collaborative. The traditional process involves physicians manually contacting the department manager or the planner to coordinate the changes. It’s challenging to manage, especially in large healthcare organizations with many departments and specialties across multiple sites.
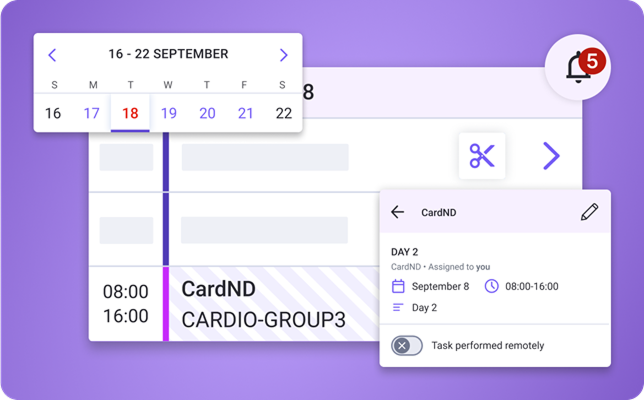
Physician scheduling solutions are software designed to simplify the process of creating and managing schedules for healthcare providers. Advanced solutions provide user-friendly interfaces for physicians to manage their schedules and communicate their availability directly, empowering physicians to take control of their agenda.
Software, like Petal Workforce Management, improves efficiency and allows for better care by promptly identifying and assigning suitable staff replacements. In turn, patients receive the care they need without disruptions. As banking software accelerates transactions, scheduling software accelerates schedule management to facilitate more efficient operations.
CHUM decreased time spent scheduling by 98% using Petal WFM.
Challenge 3: Overcoming administrative burden
Patient self-scheduling is not a panacea for scheduling problems. While healthcare technology offers tremendous potential for personalized care, studies show that self-scheduling often leads to wasted time. This is because patient judgements of their needs, such as the intensity of their problem, as well as levels of commitment to practitioners, may misalign with their physician’s best judgements.
Healthcare planners must consider multiple factors when building schedules. This includes physician availability, shift length and rotations, patient demand, and more. Each element adds complexity to the planning process, which can lead to scheduling conflicts, strained staff satisfaction, and compromised patient care.
The dramatic rise in physician burnout rates partially reflects increased administrative burden on physicians and other care providers. The need to consider multiple factors often requires manual adjustments. Further, planners must navigate the complexities of balancing physician availability, ensuring appropriate shift coverage, and accommodating patient care demands.
Fortunately, there are solutions to reduce this administrative burden and strengthen organizational efficiency. Advanced planning tools automate tasks, simplify scheduling and reduce errors. This data-driven approach streamlines the scheduling process, reducing the time and effort required compared to manual methods.
★ Did you know that Petal data is stored in Canada and secured by industry leading SOC 2 Type II protection?
For example, standardized scheduling templates incorporate specific requirements, such as preferred shift lengths, maximum consecutive work hours, and particular skills and expertise needed for specific shifts. Those templates are adaptable to meet your unique needs.
Solutions that leverage AI technology to analyze past schedules and identify allocation trends offer a level of customization specific to each healthcare department or organization. Research from the American Society of Anesthesiologists showed AI scheduling tools dramatically reduced one department’s monthly time required to create new schedules from 60–75 hours to only 14 hours
Challenge 4: Limiting communication errors
Communication plays a crucial role in effective physician scheduling. For example, communication gaps or transcription errors following a call between an assistant and a physician slows productivity. The consequences of miscommunication can be significant, leading to double bookings, overlooked shift requests, or incorrect duty assignments, negatively impacting scheduling accuracy and staff satisfaction.
In response, physicians use integrated communication systems within their scheduling solution. The integration minimizes conflicts arising from miscommunication or transcription errors, fostering a more harmonious, productive, and efficient scheduling environment for administrators and physicians. Secure, real-time access to up-to-date information allows staff members to remain informed on schedule changes, shift swaps, and updates.
Challenge 5: Supporting physician autonomy
Supporting physician autonomy in scheduling is a crucial challenge facing healthcare organizations today.
Granting physicians independence simplifies the scheduling process. This autonomy empowers doctors to determine their schedule preferences, supporting work-life balance and optimized productivity. Then, physicians have the ability to better manage their time by gaining more control over their schedules, reducing stress, and enhancing their overall job satisfaction.
- Did you know that Petal Care Escalation deploys urgent alerts via calls, SMS, secure messaging, text-to-speech, pagers, and emails?
With collaborative physician scheduling software, physicians become active contributors, improving collaboration and information accuracy and reducing conflicts. They easily update their availability, request shift swaps, or communicate scheduling preferences or conflicts. They view their schedules in real-time, receive notifications for any changes or updates, and share openly with planners and other team members.
Empowering doctors with schedule controls ultimately contributes to a more collaborative and productive work environment.
Satisfy more staff and care for more patients without using more resources
Task automation simplifies operations, enhances efficiency, and improves the overall well-being of physicians. Petal Workforce Management is your software suite to make it happen.
Petal’s physician scheduling solution enables administrators, planners and physicians to manage schedules seamlessly. Users save valuable planning time, reduce their administrative burden, and balance clinical workload. Whether it’s handling shift rotations, managing last-minute changes, or ensuring equitable workload distribution, Petal provides a comprehensive solution that aligns with the unique needs of healthcare organizations.
Effective physician scheduling is essential to collaborative ecosystems, satisfied staff, and supported patients. The challenges faced by healthcare planners can be overcome by adopting healthcare technology solutions that address each specific problem.
Are you ready for the future of physician scheduling?
Simplify your operations to save more time for patients.
- Green, Christian (2022, September 7). Stress and burnout a growing concern for healthcare leaders. MGMA. https://www.mgma.com/mgma-stats/stress-and-burnout-a-growing-concern-for-healthcare-leaders
- CMA (2022, November 15). Physician wellness: New 2021 National Physician Health Survey findings — burnout, short-staffing and an overburdened system take their toll. Canadian Medical Association. https://www.cma.ca/physician-wellness-hub/content/physician-wellness-new-2021-national-physician-health-survey-findings-burnout-short-staffing-and
- Youn, S., Geismar, H. N., & Pinedo, M. (2022). Planning and scheduling in healthcare for better care coordination: Current understanding, trending topics, and future opportunities. Production and Operations Management, 31(12), 4407–4423. https://doi.org/10.1111/poms.13867
- ASA (2022, January 28). Using AI to create work schedules significantly reduces physician burnout, study shows. American Society of Anesthesiologists. https://www.asahq.org/about-asa/newsroom/news-releases/2022/01/using-ai-to-create-work-schedules-significantly-reduces-physician-burnout
![PT_VOMBSFP_202509_EN[1]](https://www.petal-health.com/wp-content/uploads/2025/10/PT_VOMBSFP_202509_EN1.png)
![Rapport économiquepouce-non-arrière-plan(1)[1]](https://www.petal-health.com/wp-content/uploads/2025/10/Economic20report20thumb-no20background2011-768x548.png)