Key takeaways
- Lock and limit time‑off requests before building schedules to stabilize data, reduce back‑and‑forth, and produce faster, fairer schedules.
- Automate with up‑to‑date rules and equity management to create transparent, defensible shift distribution.
- Extend scheduling to rooms and resources, and drive secure, mobile adoption to improve coverage, speed up swaps, and increase access to care.
Healthcare scheduling is more than filling shifts—it’s about balancing fairness, reducing administrative load, and ensuring patients have timely access to care. Yet, many organizations still rely on manual processes that create inefficiencies, increase stress for planners, and pull clinicians away from what matters most: patient care.
The good news? Proven best practices, supported by the right technology, transform scheduling from a pain point into a strategic advantage.
Below are seven practical steps to help you streamline scheduling, improve equity, and strengthen care delivery.
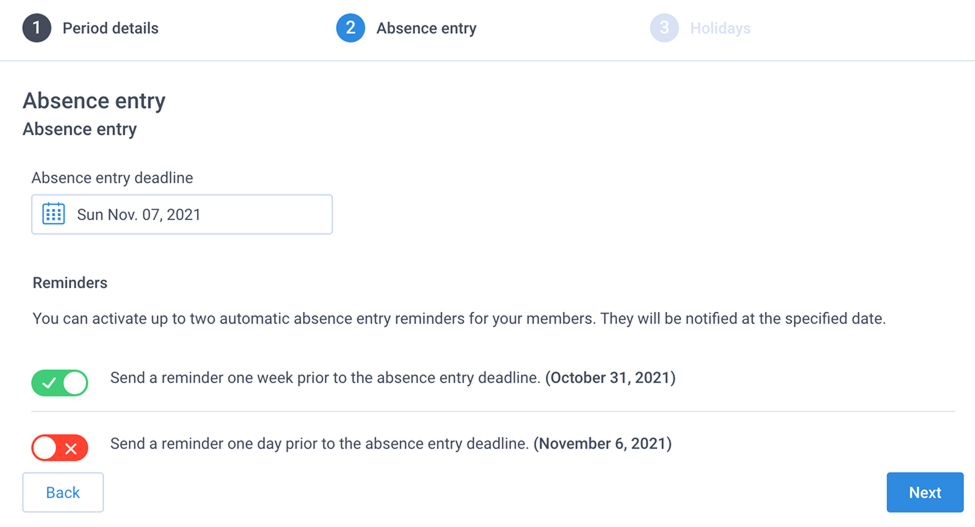
1) Lock absence entry before you build the schedule
Succeeding at scheduling starts with stable inputs. Set a clear deadline for absence submissions and lock new entries before you begin building the schedule. This simple control prevents mid‑cycle surprises and stops the churn of rework.
How to put it into practice
- Communicate the submission deadline for each upcoming schedule period.
- Turn on automated reminders inside Petal to prompt those who haven’t submitted.
- Lock absence entry on the date you shared.
- Proceed with a clean, stable dataset.
2) Set absence limits to protect coverage and equity
Unlimited or ad‑hoc absences overload planners and jeopardizes coverage. Configure absence caps that reflect service realities, whether by season, role, or service line. Setting smart limits reduces exceptions management and creates a fair, defensible framework that supports access to care.
Tips
- Use unique caps for peak periods (e.g., summer) and for the full year.
- Share the policy with your group to align expectations.
- Review utilization quarterly and adjust limits as staffing or demand evolves.
The third tip is the most challenging, as it involves limitations on physicians. Yet, more importantly, it sets collective expectations. Transparent communication about those limits shared early and often supports smoother coverage.
The result: fewer hard stops in coverage, less manual triage, and a process everyone understands.
3) Link physicians and residents for coordinated care
Residents and attending physicians both benefit from visibility into each other’s assignments. Configure physician–resident associations so both parties see linked shifts in their calendars. When a change occurs, the right people receive the right update at the right time.
Why it matters
- Streamlines supervision and teaching.
- Reduces confusion and double‑booking.
- Supports safer handoffs and team‑based care.
To begin, create the relevant shift types and ask the Petal team to configure the associations to your exact rules. Once in place, the system maintains those links automatically.
The result: quicker schedule creation due to existing rules and connections and better coordinated care from both resident and supervising physician.
4) Keep your automation script current (advanced automation users)
Automated scheduling only performs as well as the rules behind it. Any change in staffing, service requirements, or preferences deserves a rules refresh before you run your next schedule. Avoid patching with manual fixes; update the automation script so the engine reflects today’s reality.
When to update
- New hires or departures
- Changed availability patterns
- Updated service minimums or maximums
- New equity or preference rules
Petal’s scheduling specialists support script reviews and edits. A quick check‑in keeps your rules aligned and your outcomes optimal.
5) Use equity management to build trust and retention
Perceived fairness drives morale. Petal’s equity management features track distribution across nights, weekends, holidays, and high‑demand duties. With clear rules and transparent reporting, you demonstrate fairness, address outliers early, and reduce disputes.
Best practices
- Define what “fair” means in your group (weightings, rotation cadence, protected time).
- Publish the equity policy and track it.
- Review equity dashboards after each schedule and share a quick summary.
The outcome: fewer grievances, less emotional labor for planners, and a stronger foundation for recruitment and retention—directly supporting continuity and access for patients.
6) Schedule rooms and resources to unlock capacity
People scheduling solves only part of the access challenge. Extend planning to operating rooms, clinics, procedure rooms, and specialized equipment. Align the right clinician with the right room and resources at the right time. When resource scheduling lives inside the same platform, you maximize throughput and reduce idle time.
Practical moves
- Prioritize rooms based on backlog, clinical urgency, and case complexity.
- Tie block time to performance and reallocate unfilled capacity earlier.
- Use standardized rules for escalation and release to improve fill rates.
This approach increases available appointments, shortens wait lists, and promotes on‑time starts—direct wins for access to care.
7) Drive full team adoption—especially on mobile
A great schedule loses impact when updates live in inboxes or side chats. Get every clinician, coordinator, and stakeholder onto the Petal platform and mobile app. Centralized communication and real‑time notifications reduce errors and accelerate swaps.
Enable the behaviours you want
- Offer a short training session focused on common tasks (absences, swaps, viewing the team calendar).
- Set expectations: all changes flow through Petal; no shadow spreadsheets.
- Encourage mobile usage for instant visibility and faster response times.
- Loop in the phone center and residents so everyone sees the same source of truth.
The result: fewer missed messages, fewer coverage gaps, faster problem resolution, and more hours preserved for patient care.
Putting it all together
Modern scheduling reduces administrative burden and expands access when it follows a few clear principles:
- Stabilize inputs (lock and limit absences).
- Codify fairness (equity rules, transparent tracking).
- Automate with intention (keep scripts current, avoid manual solutions).
- Plan the whole system (people and rooms/resources).
- Centralize communication (platform + mobile adoption).
These practices remove friction from the workday, protect clinician time, and keep services responsive to patient demand. Less time spent chasing updates means more time with patients.
Next steps
- to review your absence policy, equity rules, and automation script.
- Enable resource scheduling for operating rooms or procedure spaces to unlock latent capacity.
- Host a 30‑minute team refresher to drive full adoption and eliminate shadow workflows.
Ready to reduce admin load and increase access to care? Let’s optimize your schedule and give your team more time for patient care.
![PT_VOMBSFP_202509_EN[1]](https://www.petal-health.com/wp-content/uploads/2025/10/PT_VOMBSFP_202509_EN1.png)
![Rapport économiquepouce-non-arrière-plan(1)[1]](https://www.petal-health.com/wp-content/uploads/2025/10/Economic20report20thumb-no20background2011-768x548.png)